Gastric cancer patients recover faster and have less pain after surgery
- Seoul National University Hospital, ‘Enhanced Recovery After Surgery Program (ERAS)’ proves effectiveness through randomized clinical trial
- Quality of Recovery index (QoR-15K) average ↑16 points, pain and narcotic analgesic use reduced, hospitalization period shortened
Researchers at Seoul National University Hospital (SNUH) implemented the Enhanced Recovery After Surgery (ERAS) program for patients undergoing laparoscopic or robotic gastric cancer surgery. They found that the quality of postoperative recovery significantly improved. This study was conducted as a prospective randomized controlled clinical trial, which confirmed that recovery quality improved, pain levels decreased, the usage of narcotic analgesics was reduced, and the length of hospital stays was shortened.
Gastric cancer is the fourth most common cancer in Korea. Radical resection remains the primary treatment, especially in early-stage cases or when lymph node metastasis is present. Although most surgeries are now performed using minimally invasive techniques such as laparoscopy or robotic surgery, patients still experience significant postoperative challenges, including pain and impaired gastrointestinal function.
ERAS is an evidence-based, multidisciplinary approach designed to promote fast and safe recovery before and after surgery. While it has become a standard in Europe for various cancers—including colorectal, hepatobiliary, and lung cancers—its effectiveness for minimally invasive gastric cancer surgery, which is common in Asia, has not been conclusively demonstrated.
Accordingly, the research team of Professor Park Do Joong of the Department of Gastroenterology and Professor Lee Ho-Jin of the Department of Anesthesiology and Pain Medicine at SNUH developed an ERAS program dedicated to minimally invasive gastric cancer surgery tailored to the domestic clinical environment. To evaluate its effectiveness, a prospective randomized controlled clinical trial was conducted on a total of 92 gastric cancer patients who underwent laparoscopic or robotic distal gastrectomy from February 2023 to May 2024. The patients were divided into the ERAS group (45 patients) and the conventional treatment group (47 patients) and received treatment.
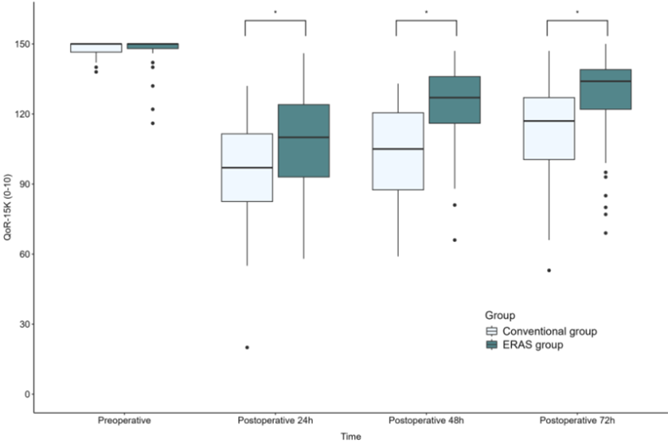
[Figure] The ERAS group (green) achieved an average QoR-15K score 16 points higher than the conventional treatment group (white) over the first three days post-surgery, indicating a significant improvement in recovery quality."
The ERAS program implemented includes: ▲minimizing fasting before and after surgery, including preoperative carbohydrate drinks, ▲ultrasound-guided abdominal nerve block, ▲multimodal analgesia incorporating non-narcotic medications, and ▲prevention of nausea and vomiting. This approach offers a safer, evidence-based integrated recovery strategy, shifting away from traditional reliance on narcotic painkillers.
The main evaluation index was the QoR-15K score (Korean version of the Quality of Recovery Assessment Questionnaire, total score 0–150 points) measured 24, 48, and 72 hours after surgery. The QoR-15K consists of 15 questions that evaluate the postoperative recovery status in five areas: physical comfort, emotional state, physical independence, psychological support, and pain management. The research team judged a score difference of 8 points or more as a clinically meaningful improvement according to existing literature. As a result, the ERAS group recorded an average QoR-15K score 16 points higher than the conventional treatment group (95% confidence interval: 8.9–23.0, P<0.001), showing statistically and clinically significant improvement in the quality of postoperative recovery.
The ERAS group also showed better recovery overall in secondary evaluation indicators. The pain score when coughing 48 hours after surgery was 5 points on average in the conventional treatment group, while it was 3 points in the ERAS group. The amount of narcotic analgesics used 72 hours after surgery decreased by approximately 40% from the conventional average of 1,260 μg to 780 μg in the ERAS group. The I-FEED score, which reflects the recovery of intestinal function, improved by 3 points on average in the conventional treatment group and 1 point in the ERAS group 24 hours after surgery. In addition, the time to first gas discharge was 21 hours faster in the ERAS group. The total length of hospital stay was also 1 day shorter in the ERAS group on average.
The research team concluded that the ERAS program not only enhances recovery quality for gastric cancer surgery patients but also offers a safer, more efficient alternative to traditional practices centered on prolonged fasting and narcotic analgesics. Shorter hospital stays may also reduce socio-economic costs.
Professor Lee Ho-Jin (Department of Anesthesiology and Pain Medicine, first author) said, “In Korea, excessive fasting before and after surgery and pain management centered on narcotic analgesics are still widely used. However, through this study, we confirmed that a more evidence-based perioperative management strategy is effective,” and “We hope to contribute to establishing new surgical management standards that emphasize the quality of recovery in the future.”
Professor Park Do Joong (Department of Gastroenterology, corresponding author) said, “This clinical trial is an important study that proved the effectiveness of an ERAS program specialized for gastric cancer patients through a randomized comparative method.” He added, “A multi-institutional joint study is currently underway with 10 domestic hospitals participating, and we will also work to establish a policy foundation so that this program can become the standard treatment guideline for gastric cancer surgery in Korea.”
This study was conducted as part of the Cancer Conquest Promotion Research and Development Project supported by the Ministry of Health and Welfare and the National Cancer Center, and the results were published in the latest issue of the international academic journal ‘International Journal of Surgery’.
[From left] Professor Park Do Joong (Department of Gastroenterology) and Professor Lee Ho-Jin (Department of Anesthesiology and Pain Medicine) at SNUH