Stroke awareness in Korea has improved: in-depth understanding has declined
- Seoul National University Hospital announces results of nationwide survey comparing public stroke awareness levels in 2009 and 2023
- Stroke warning symptoms recognition increases from 61.5% to 74.4%, recognition of 2 or more risk factors decreases from 51.4% to 40.2%
- Those under 40 years old and those with unhealthy lifestyle habits have a lower probability of appropriately responding to stroke symptoms
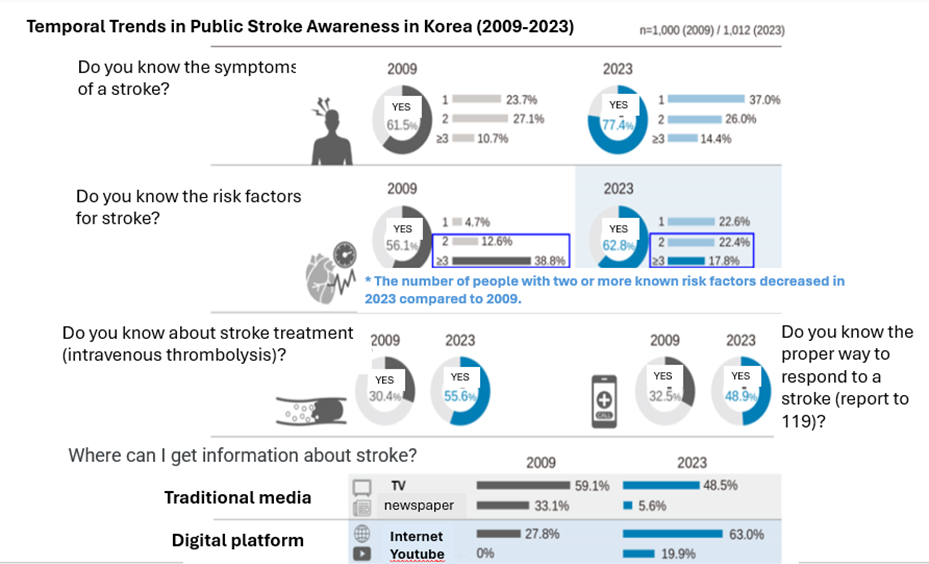
[Figure] Temporal Trends in Public Stroke Awareness in Korea (2009-2023)
On May 16th, Professor Jung Keun-Hwa of the Department of Neurology at Seoul National University Hospital (SNUH) and Professor Lee Eung-Joon of the Public Clinical Department announced the results of a nationwide survey comparing the level of stroke awareness between 2009 and 2023. According to the study, the level of public stroke awareness in Korea has improved overall, but the in-depth understanding of various risk factors has decreased. In addition, the rate of information acquisition through digital platforms has increased rapidly, and the rate of intravenous thrombolysis (IVT) awareness and emergency response has increased but is still inadequate. These results suggest that the overall level of stroke awareness has improved, but that people remain insufficiently informed, and the digital information gap still remains a problem.
Stroke is a disease in which acute brain damage occurs in the brain due to blockage or rupture of a cerebral blood vessel and is one of the major causes of death. The incidence rate continues to increase as the elderly population grows, and as of 2021, the domestic stroke incidence rate was 212.2 cases per 100,000 people, with more than 1,500 cases occurring among those aged over 80. Major symptoms include paralysis of one arm or leg, speech impairment, facial distortion, and decreased consciousness. If a stroke is suspected, it is important to immediately call 119 and promptly seek treatment. Risk factors for stroke include high blood pressure, diabetes, hyperlipidemia, heart disease, and family history of stroke, and managing these risk factors is essential for prevention.
However, in Korea, if symptoms are mild, hospital arrival is often delayed due to a lack of timely emergency treatment, and the rate of acute care remains low. In particular, in order to perform active acute treatment such as intravenous thrombolysis, it is essential to shorten the delay in hospital arrival. Previous studies have reported that hospital arrival delays are becoming longer, especially when stroke symptoms are mild. This can postpone acute treatment and ultimately worsen stroke outcomes. To address this issue, the research team analyzed changes in public awareness of stroke and changes in information-acquisition channels and sought to establish basic data for developing effective educational strategies in the future.
This study is a nationwide survey comparing the level of stroke awareness at two points in time, 2009 and 2023. In 2009, a telephone survey was conducted with 1,000 people, and in 2023, an online survey was conducted with 1,012 people. Both surveys ensured national representation through proportional quota sampling based on demographics and were conducted using stratified sampling methods considering gender, age, and region. The survey evaluated awareness of stroke warning symptoms, risk factors, treatment methods, and appropriate responses when symptoms occur.
The study revealed that awareness of stroke warning symptoms rose from 61.5% in 2009 to 77.4% in 2023. However, awareness of two or more stroke risk factors decreased from 51.4% to 40.2%. Notably, this decline in awareness was particularly significant among individuals without vascular risk factors, indicating that there still exists a group that is vulnerable to collecting information.
In addition, in 2023, awareness of intravenous thrombolysis significantly increased from 30.4% to 55.6%, and the proportion of those who selected 119 when stroke symptoms occurred also increased from 32.5% to 48.9%. The analysis results showed that awareness of intravenous thrombolysis (adjusted odds ratio [aOR] = 1.54) and recognition of two or more warning symptoms (adjusted odds ratio [aOR] = 1.43) were significantly related to an increased probability of reporting to 119. In other words, people who are aware of intravenous thrombolysis and recognize two or more warning symptoms are more likely to report to 119 when stroke symptoms occur.
On the other hand, those under 40 years of age and those with unhealthy lifestyle habits (smoking, binge drinking, lack of exercise, etc.) were less likely to respond appropriately when stroke symptoms occurred. This suggests that these groups lack awareness of stroke and emergency response behavior.
The route through which health information is acquired has changed significantly over the past 14 years. The proportion of information acquisition through TV decreased from 59.1% in 2009 to 48.5% in 2023, while the proportion of information acquisition through digital media such as the Internet (27.8% → 63.0%) and YouTube (0% → 19.9%) increased significantly.
Professor Jung Keun-Hwa explained, “This is the first large-scale study to assess changes in stroke awareness at two points in time (2009 and 2023), and although overall awareness has improved, the depth of information has decreased.”
He added, “Going forward, it is crucial to develop differentiated educational strategies tailored to age groups, health behaviors, and underlying conditions, and to create reliable digital-based educational content.”
This study was conducted with the support of the Korea Centers for Disease Control and Prevention, the National Institute of Health, the Korean Stroke Society, and the Central Cardiovascular Disease Center, and the results were published in the latest issue of the Journal of the American Heart Association.
[Pictures from left] Professor Jung Keun-Hwa from SNUH Department of Neurology and Public Health Clinical Professor Lee Eung-Joon