Early treatment following the onset of adult MOG antibody disease (MOGAD) is effective in preventing long-term relapses and reducing MOG antibody levels in the body.
- MOGAD leads to inflammation in the central nervous system, such as optic neuritis… More than half of adult patients experience a relapse.
- An analysis of treatment timing and relapse risk was conducted on 240 adult patients with first-onset MOG antibody disease.
- The results indicated that the group treated for more than 14 days had a 2.6 times higher risk of relapse compared to the group treated for less than 4 days.
A domestic research team suggested a treatment strategy to improve the long-term prognosis of adult patients with Myelin Oligodendrocyte Glycoprotein Antibody Disease (MOGAD), a disease with frequent relapses. The research results showed that acute treatment within 4 days of the first MOGAD onset can lower the risk of relapse of the disease and help suppress the autoimmune response.
A joint research team, Professor Kim Sung-Min from Seoul National University Hospital(SNUH) Department of Neurology, Professor Kim Seong-Joon & Prof Jung Jae Ho from Department of Ophthalmology, and Professor Kwon Young Nam & Shin Ha Young from Yonsei University Severance Hospital Department of Neurology, announced the results of an analysis of the correlation between the timing of acute treatment and long-term prognosis in adult patients with MOGAD who visited 14 domestic hospitals from November 2009 to August 2023.
MOGAD is a rare inflammatory disease of the central nervous system resulting from an autoimmune reaction, causing optic neuritis, myelitis, and encephalitis, which can lead to visual impairment and movement disorders. Recently, as a MOG antibody test method specific to this disease has been developed, its diagnostic prevalence is also increasing.
In the early stages of MOGAD, ‘acute-stage treatment’ using steroids, etc. is used. Afterwards, ‘immunosuppressant treatment’ is maintained for a long period to prevent relapse. Recent research indicates that initiating acute-stage treatment sooner reduces the risk of relapse. However, there has been a notable lack of studies analyzing the relationship between early treatment policies and long-term prognosis in adult patients, over half of whom experience relapse.
The research team divided adult patients with MOGA for the first time into ▲early (within 4 days) ▲intermediate (5-14 days) ▲late (after 15 days) treatment groups according to the time of starting acute treatment and monitored the risk of relapse for more than 1 year.
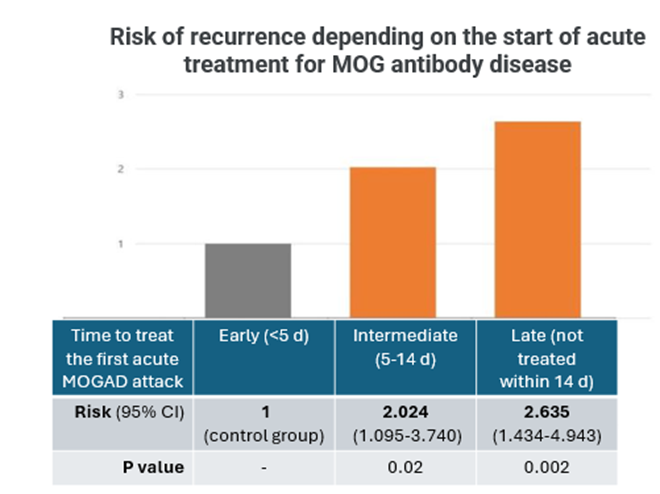
[Graph] Analysis of relapse risk according to the time to start treatment for MOG antibody disease in the acute attack phase. The risk of relapse in the intermediate and late treatment groups increased by 2.02 and 2.64 times, respectively, compared to the early treatment group.
The analysis results showed that the risk of relapse increased as treatment was delayed. Compared to the early treatment group, the risk of relapse in the intermediate and late treatment groups increased by 2.02 and 2.64 times, respectively.
In addition, it was shown that early acute-stage treatment could lower the risk of relapse regardless of long-term immunosuppressive treatment. It was confirmed that patients who did not receive long-term immunosuppressive treatment but received early acute treatment had a lower risk of relapse than patients who received intermediate and late treatment.
Additionally, the research team analyzed the correlation between the timing of acute treatment and serum MOG antibodies that are produced due to autoimmune reactions. As a result, the early treatment group was about 7 times more likely to lose this antibody than the late treatment group, indicating that early acute treatment plays an important role in suppressing autoimmune reactions and eliminating MOG antibody reactions, which are major markers of the disease.
Meanwhile, long-term immunosuppressive treatment was not associated with the loss of MOG antibodies but was confirmed to be an independent factor that lowers the risk of relapse. Therefore, the research team explained that both acute treatment and long-term immunotherapy are effective in preventing long-term relapse.
Professor Kim Seong-Min (Neurology) said, “Through this study, we confirmed that early acute treatment is an important factor that can increase the possibility of a complete cure for MOGAD,” and “If MOGAD is actively diagnosed early and acute treatment is administered quickly, it will help suppress relapse and autoimmune reactions.”
The results of this study were published in the American neuroscience journal ‘JAMA Neurology.’
[Pictures from left] Professor Kim Sung-Min from Seoul National University Hospital Department of Neurology, Professor Kim Seong-Joon & Professor Jung Jae Ho from Department of Ophthalmology, and Professor Kwon Young Nam & Professor Shin Ha Young from Yonsei University Severance Hospital Department of Neurology