Seoul National University Hospital and Seoul National University develop a biomarker to predict treatment of acute myeloid leukemia
Development of a ‘high-performance companion diagnostic biomarker’ using the single-molecule pull-down and co-immunoprecipitation technology... Customized treatment becomes possible
- Uncovered the mechanism of action of ABT-199 and confirmed that patients’ anti-cancer drug responsiveness can be predicted with high accuracy
- Prediction accuracy of up to 94% at the in vitro level... 100% sensitivity and 83.3% specificity were confirmed in clinical trials.

A joint research team from Seoul National University Hospital and Seoul National University announced a groundbreaking study opening the possibility of customized treatment for patients with acute myeloid leukemia (AML). The research team used new technology to identify the mechanism of action of the ABT-199 targeted anticancer drug and developed a ‘high-performance companion diagnostic biomarker’ that can predict the treatment response of individual patients with high accuracy. The results of this study were published in the latest issue of the world-renowned academic journal ‘Nature Biomedical Engineering (IF: 29.2)’.
Seoul National University Hospital Department of Hematology and Oncology Professor Koh Young-il and Professor Byun Ja Min, Seoul National University Department of Life Sciences Professor Yoon Tae-Young (Researcher Chun Changju), and the joint research team of PROTEINA announced on August 6th that they developed a high-performance companion diagnostic biomarker that can predict the therapeutic effect of the ABT-199 targeted anticancer drug by analyzing the interaction between the BCL2 protein and other proteins using single-molecule pull-down and co-immunoprecipitation (SMPC) technology.
Acute myeloid leukemia (AML) is a type of blood cancer in which abnormal white blood cells in the blood or bone marrow rapidly proliferate and interfere with the production of normal blood cells. The selection of a rapid and effective treatment is very important. BH3 mimetics are drugs that induce the death of cancer cells by targeting the BCL2 protein. In particular, the targeted anticancer drug ‘ABT-199 (Venetoclax)’ has shown high performance in the treatment of AML.
However, not all patients experience the same treatment effects, and resistance may develop after temporary remission, so a method to predict the effect of ABT-199 in advance was needed.
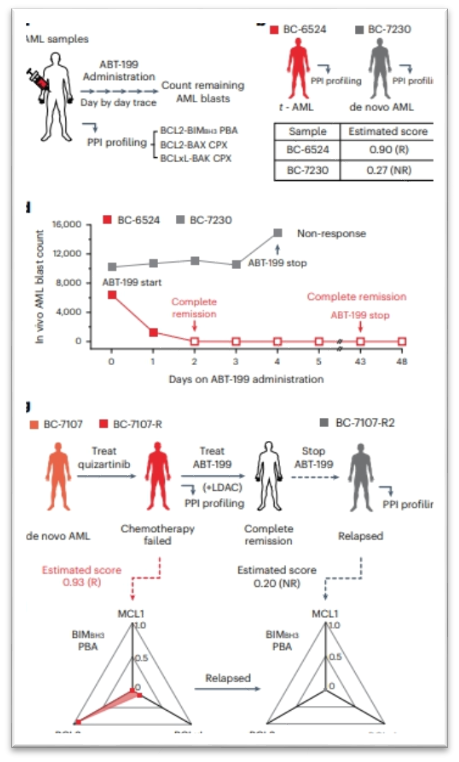
[Figure] Blood samples confirmed that PPI profiling data related to the BCL2 protein group can accurately predict ABT-199 (Venetoclax) responsiveness in leukaemia patients.
The research team developed a technology to quantitatively detect 22 different protein-protein interaction (PPI) signals by analyzing about 30,000 cells using single-molecule pull-down and co-immunoprecipitation (SMPC) and single-molecule fluorescence imaging techniques. These techniques allow them to accurately measure how various proteins interact with each other.
The research team confirmed that ABT-199 selectively binds to the BCL2 protein and degrades the BCL2-BAX complex. Through this process, the activated BAX protein induces the death of cancer cells. They clearly elucidated the primary mechanism by which ABT-199 kills cancer cells.
The research team then obtained multidimensional PPI profile data from 32 AML patient samples and analyzed the correlation with drug response at the in vitro level. As a result, they identified major protein complexes that affect the sensitivity (how well it works) and resistance (how much it resists) of ABT-199. In particular, they confirmed that the BCL2-BAX complex is related to the sensitivity of ABT-199, and the BCLxL-BAK complex is related to the resistance.
Based on this data, the research team developed a ‘high-performance companion diagnostic biomarker’ that can predict the drug response of ABT-199 in individual AML patients. This biomarker can predict with high accuracy whether ABT-199 will be effective by observing how specific PPI signals change in the patient’s cells.
The research team tested the prediction accuracy of the developed biomarker at the in vitro level. As a result, they found a prediction accuracy (AUC-ROC) of up to 94%, which is sufficient for clinical application. In a clinical test targeting 10 actual AML patients, it successfully predicted the anticancer drug response of 9 people, showing a sensitivity of 100% and a specificity of 83.3%. This confirmed that it can predict the anticancer drug response of patients with high accuracy.
Professor Yoon Tae-Young (Life Sciences) of Seoul National University said, “The single-molecule coimmunoprecipitation (SMPC) technique is a tool that can precisely measure protein-protein interactions (PPIs) in various samples,” adding, “This technology is expected to open a new path for molecular diagnosis by understanding complex protein interaction networks.”
Professor Koh Young-il (Hematology and Oncology) of Seoul National University Hospital stated the significance of the study, saying, “This study is a meaningful achievement that highlights the importance of ABT-199 (Venetoclax) therapy in acute myeloid leukemia, where response prediction biomarkers were previously lacking.” He also said, “This study based on PPI profiling will greatly contribute to the development of precision medicine for acute myeloid leukemia in the future.”

[Pictures from left] Prof Koh Youngil & Prof Byun Ja Min from Dept of Hematology and Oncology, SNUH and Prof Yoon Tae-Young & Researcher Chun Changju from Dept of Biosciences, SNU