Hematopoietic Stem Cell Transplantation from Haploidentical Related Donors has shown similar treatment results compared with Transplantation from Matched Unrelated Donor
- There is no difference in the survival rate and complication rate, and treatment outcome between HRD HSCT and MUD HSCT treated patients
- The possibility of successful hematopoietic stem cell transplantation has increased for those patients who are unable to find an appropriate Matched Unrelated Donor (MUD)
Our results confirmed that pediatric acute leukaemia patients who need Hematopoietic Stem Cell Transplantation (HSCT) showed similar treatment outcomes when comparing patients who received matched unrelated donor (MUD) HSCT with those who had a haploidentical related donor (HRD) HSCT from his/her family.
For many patients who were unable to receive a hematopoietic stem cell transplant because they could not find an appropriate matched unrelated donor, HRD HSCT is expected to be a new viable alternative.
On April 23, Professor Kang Hyung Jin and Hong Kyung Taek’s team, the Department of Pediatrics at Seoul National University Hospital, published the results of a comparative analysis of treatment outcomes between the HRD HSCT group and the MUD HSCT group. Both groups underwent graft-versus-host disease prophylaxis after administration of appropriate doses of anticancer drugs (Busulfan) to each individual.
Hematopoietic stem cell transplantation (HSCT) is an essential treatment for patients with high-risk acute leukaemia. However, up until now there has been a limiting factor that generally good outcomes following this treatment could only be expected when transplantations were received from a sibling or matched unrelated donor (MUD) whose histocompatibility antigens (antigens recognized as the same type in the immune response) matched the patient’s.
However, due to recent low fertility rates, it has become more difficult to find sibling donors, and the probability of matching the histocompatibility antigens even with siblings is already only 25%. Therefore, if the patient is an only child or their sibling’s histocompatibility antigens do not match theirs, an appropriate unrelated donor must be found through a hematopoietic stem cell bank. However, the probability of finding an unrelated donor with a matching histocompatibility antigen is also low, about 50%. Cord blood transplantation was sometimes performed, but it was difficult because bone marrow engraftment was often slow and there were many complications of infection.
In recent years, the numbers of HRD HSCT have been gradually increasing. However, there have been few studies on children and adolescents comparing the treatment outcomes between HRD HSCT and MUD HSCT so far.
The research team compared and analyzed the treatment outcomes of high-risk pediatric acute leukaemia patients from a ▲HRD HSCT group (35 patients) and ▲MUD HSCT group (45 patients), from January 2013 to April 2020.
As a result, the survival rate of patients who underwent HRD HSCT with only half histocompatibility antigen matching was 88.6%. On the other hand, the survival rate of patients who received MUD HSCT with histocompatibility antigen matched was confirmed to be 83.7%. The data showed that the success of the therapeutic effect between HRD HSCT and MUD HSCT was fairly close.
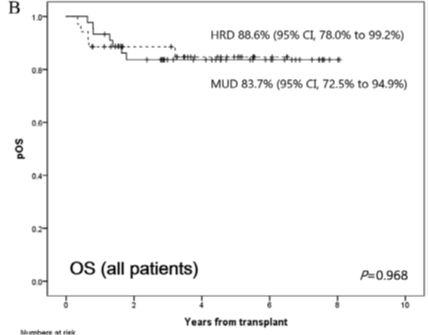
(Figure 1) Comparing overall survival rates: Haploidentical Related Donors (HRD) HSCT VS Matched Unrelated Donors (MUD) HSCT
In addition, the cumulative incidence of grade II-IV acute or chronic graft-versus-host disease (GVHD), a complication, was 2.9% and 11.4% respectively in the HRD HSCT group, which was lower compared to the MUD HSCT group (8.9% and 18.3%, respectively).
In particular, the survival rate of acute myeloid leukaemia patients was higher in the HRD HSCT group (93.8%) than in the MUD HSCT group (85.6%), showing excellent treatment results.
The research team explained the reason why HRD HSCT showed comparable treatment results to that of MUD HSCT was by combining the administration of anticancer drugs (Busulfan) at personalized concentration together with [Cyclophosphamide] administration after transplantation which has made the treatment process more safe and effective.
Above all, the research team emphasized that the lower incidence of GVHR and the excellent survival rate of patients with acute myeloid leukaemia compared to conventional unrelated transplants are encouraging results.
Professor Kang Hyoung Jin said, "We expect that the results of this study will serve as a basis for effective and safe HRD transplantations in cases where it is difficult to receive HSCT due to the lack of an appropriate donor or if haploidentical related donors (HRD) HSCT are needed for patients whose transplantations have been delayed."
This research was published in the ‘American Society for Transplantation and Cellular Therapy Journal’, an authoritative journal related to hematopoietic stem cell transplantation.
(Picture 1) From left: SNUH, Prof Kang Hyoung Jin & Prof Hong Kyung Taek